Breastfeeding is a beautiful journey that nourishes your baby with the perfect blend of nutrients and antibodies. But for busy moms, pumping allows for flexibility and convenience, ensuring your baby receives the benefits of breastmilk even when you’re not there.
Whether you’re a seasoned pumping pro or just starting out, mastering the process of pumping, storing, thawing, and feeding breastmilk empowers you to confidently navigate your breastfeeding journey. Here’s your comprehensive guide:
Pumping Essentials:
Find Your Rhythm: Establish a pumping routine that works for you. It could be several short sessions throughout the day or longer stretches that fit your schedule. Consistency is key to maintaining milk supply.
Choosing Your Pump: A high-quality breast pump makes a world of difference. Hygeia Health offers a comfortable, efficient, and quiet hospital-grade pump that is free to many through insurance. Consider your needs – portability for on-the-go pumping or a hospital-grade option for frequent pumping sessions.
Perfect Latch & Positioning: Proper positioning and latch ensure optimal milk flow and prevent discomfort. Your baby’s mouth should be wide open, with their chin and lower lip flanged outward. Their tongue should be positioned over a large portion of your nipple and most of the darker area around your nipple, called the areola). This ensures they get enough milk and prevents nipple pain for you. If you’re unsure about your latch, don’t hesitate to ask a lactation consultant for help.
Storing Liquid Gold: Safeguarding Your Breast Milk
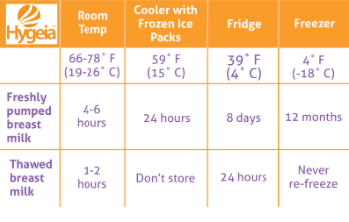
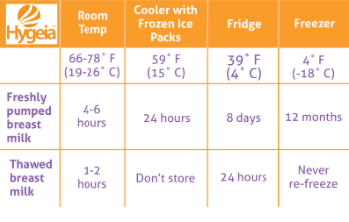
Fresh is Best: Freshly pumped breast milk can be stored at room temperature (up to 77°F) for up to 4 hours. This is ideal for short outings or pumping between nursing sessions.
Refrigerator Storage for Later: For longer storage, refrigerate breast milk in the back of the refrigerator where the temperature is most stable. Properly stored milk can last up to 4 days.
Deep Freeze for Long-Term Storage: Breast milk can be stored in the deep freezer (at 0°F or below) for up to 12 months. However, milk quality can degrade over time. Label containers with the date to ensure you use the oldest milk first.
Adding to your Storage: Small amounts of expressed milk may be added to the same refrigerated container or even a frozen container. The key is that the milk you want to add is cooled in the fridge beforehand. Don’t add body-temperature milk to cooled or already frozen milk.
Hygeia’s Storage Solutions: Invest in high-quality breast milk storage bags or containers. Hygeia Health offers a range of leak-proof, BPA-free storage options to keep your precious milk safe, including a cooler bag for temporary storage on the go.
Thawing Treasures: Warming Up Breast Milk Safely
Never Microwave: Don’t even think about it. Not only does microwaving destroy nutrients in breast milk but it can also create hot spots that could burn your baby’s mouth.
Gradual Thawing: The safest method is to thaw frozen breast milk in the refrigerator overnight or generally 12 hours. For quicker thawing, place the sealed milk bag or container in a container of lukewarm water, but never in boiling water. This kind of heat can damage the nutrients. It is also important to not let it thaw at room temperature.
Temperature Check and mixing: Before feeding, test a drop of milk on the inside of your wrist to ensure it’s lukewarm, not hot. Be sure to swirl the milk in the bag or bottle as the milk can separate during storage and you want to blend all the fats.
Limited window: Once you’ve thawed milk and left it at room temperature, you want to feed it to your baby within two hours. If that doesn’t happen, do not refreeze the milk. It’s time to pitch.
Feeding Time! Delivering the Goodness
Room Temperature or Chilled?: Either is fine! Breast milk can be fed to your baby at room temperature or chilled. Some babies may even prefer cooler milk. You can also warm the milk to body temperature but it’s not necessary.
Fresh vs. Thawed: If possible, prioritize using fresh or refrigerated breast milk over thawed milk. Thawed milk may have a slightly different taste or smell. It’s still perfectly safe for your baby; however, it will store longer and you can’t refreeze it once thawed, so save it for later.
Bottles and Nipples: Choose bottles designed for breastfed babies to help prevent nipple confusion. Experiment with different nipple types to find one your baby takes comfortably.
Hygeia’s Feeding Accessories: Hygeia Health offers a variety of bottle and nipple options to ensure a smooth transition between breast and bottle feeding.
Embrace the Journey with Hygeia Health
Juggling motherhood and breastfeeding can be demanding, but pumping empowers you to provide your baby with the irreplaceable benefits of breast milk. Hygeia Health is here to support you every step of the way.
We offer a convenient insurance-covered breast pump program to eligible mothers. Our hospital-grade pump is designed for comfort, efficiency, and portability, making it perfect for busy moms.
Click here to apply for your free breast milk pump today!
With the right knowledge, tools, and support system, you can confidently navigate pumping, storing, thawing, and feeding breast milk. Happy pumping, mamas!

September is Neonatal Intensive Care Awareness Month (NICU Awareness), a time to recognize the incredible strength and resilience of NICU families. For mothers of NICU babies, breastfeeding can be a source of comfort, connection, and nourishment.
Challenges Faced by NICU Moms
NICU moms often face unique challenges in all aspects of mothering a newborn, but specifically, breastfeeding a NICU baby can be particularly difficult. These challenges may include:
Separation from their baby: Being unable to hold and feed baby can be emotionally taxing.
Pumping challenges: Maintaining milk supply while baby is in the NICU can be physically demanding.
Stress and anxiety: The stress of having a baby in the NICU can impact a mother’s milk supply as well as the overall ability to breastfeed.
The Benefits of Breastfeeding a NICU Baby
Despite these challenges, breastfeeding a NICU baby offers numerous benefits and is still very possible. Some of these benefits include:
Colostrum: The first milk produced after birth is rich in nutrients and antibodies that can help protect your baby from infections. While baby may not be able to latch, a mom can pump and the colostrum can still nourish baby.
Reduced risk of infections: Breast milk contains antibodies that can help protect your baby from infections, which are common in NICU babies.
Improved growth and development: Breast milk is specifically designed to meet your baby’s nutritional needs and can help promote healthy growth and development, which are all the more necessary in premature births and NICU babies in general.
Stronger bond: Breastfeeding can help you bond with your baby, even if they are still in the NICU and you cannot have skin-to-skin contact.
Support NICU Moms
Supporting a mother of a NICU baby can make a world of difference. By offering your support, you can help a NICU mom feel less alone and more empowered to care for her baby. Here are a few ways you can offer your support:
Be there for her: First and foremost, offer emotional support, a listening ear, and words of encouragement.
Help with practical tasks: Helping with what seem like simple household chores, errands, or childcare for older children can make a world of difference to a stressed NICU mom.
Respect her feelings: Understand that she may be feeling stressed, anxious, or overwhelmed. Avoid making assumptions or offering unsolicited advice.
Connect her with resources: While you do have to be careful about unsolicited advice, it can be helpful to be sure she is connected with information about local support groups, lactation consultants, or other resources that can help her.
Celebrate her strength: No matter how small, take time to acknowledge her resilience and the challenges she is facing. Let her know that you appreciate her strength and courage.
How Hygeia Health Can Help
At Hygeia Health, we understand the unique challenges faced by NICU moms and are here to give the best support.
Support resources: We offer resources and support to help NICU moms on their breastfeeding journey. Our website provides information on breastfeeding and pumping, and our customer service team is available to answer your questions.
Lactation assistance: Access an expert anytime, anywhere for assurance and support on your breastfeeding journey. We partner with Nest Collaborative to provide virtual breastfeeding consults covered by most insurance plans at no cost to you.
Get a free breast pump: We believe that every mother should have access to the tools and support they need to breastfeed their baby. That’s why we offer a free breast pump to NICU moms through our NICU Mom Support Program. Our high-quality breast pumps are designed to make pumping easier and more efficient, allowing you to focus on bonding with your baby.
Let’s work together to support NICU families and celebrate the incredible strength and resilience of these amazing mothers.

Newborn cuddles and breastfeeding bliss – that’s the dream, right? The breastfeeding first week sets the stage for your journey, and it can feel overwhelming. But don’t worry, mama, we’ve got your back! This guide will break down each day, offering tips and tricks for those precious early feedings.
Day 1 & 2: Colostrum Power!
Capture the Golden Hour: Your baby is going to be ready to eat upon arrival so take advantage! That first hour outside the womb is the perfect time to let baby’s natural instincts take over and find a perfect latch. Can’t take advantage of the “golden hour”? No worries. Just try to feed your baby as soon as possible.
Focus on Colostrum: In the first few days after birth, your body produces colostrum, a thick, yellowish liquid often called “liquid gold.” It may seem like a small amount, but it’s packed with antibodies to jumpstart your baby’s immune system. This “first milk” is perfectly designed for your newborn’s tiny tummy, promoting healthy gut development and even acting as a natural laxative. Learn more about colostrum in this post.
Frequent Skin-to-Skin Contact: Focus on skin-to-skin contact during these early feedings. This closeness not only helps regulate your baby’s temperature but also strengthens the emotional bond between you and your little one.
Feeding Cues: Your newborn’s feeding cues can be subtle at first, but look for signs like rooting, sucking motions, or fussiness. Aim for frequent, on-demand feedings, allowing your baby to determine how much milk they need. This frequent suckling stimulates your body to produce more milk, a process known as supply and demand.
Day 3 & 4: Latching Like a Pro
Mastering the Latch: Your nurses or the hospital Lactation Consultant may have helped you with latching initially, but you’ll want to focus on properly latching yourself. Your baby’s mouth should be wide open, with their chin and lower lip flanged out. Their tongue should be positioned over a large portion of your nipple and most of the areola.
Transitioning to milk: You will soon notice your milk begin to “come in,” which can feel full or tingly in your breasts. This is a good sign! Your body will produce a lot more milk than it did colostrum, so don’t be surprised. If you experience any pain or discomfort during feeding, don’t hesitate to seek help from a lactation consultant (IBCLC).
First outpatient appointment: You will likely have your first outpatient appointment scheduled before you even leave the hospital. Your doctor will check in on things like feedings and diaper changes, as well as baby’s measurements. This is the perfect time to address your questions and concerns.
Day 5 & 6: Finding Your Rhythm:
Feeding Routine: You’ve likely developed some type of feeding routine, but keep in mind that newborns still have small stomachs and need to eat frequently. Be prepared for 8-12 feedings or more in a 24-hour period.
Finding a Rhythm: Your feeding routine may be demanding but your body will be adjusting to its feeding duties. Your nipples should feel some relief from any initial tenderness and you should also be gaining confidence in latching. This should give you the opportunity to experiment with new feeding positions.
Hello Hormones: It’s quite possible that you’ll feel everything from sadness and overwhelm to joy in a matter of moments. It’s normal, thanks to hormones; however, postpartum depression and postpartum anxiety are also a common concern. Familiarize yourself with the signs of both and don’t be scared or ashamed to take it to your OB, MD or Lactation Consultant for the support you need.
Day 7: 1 Week!
Celebrate Your Success: You’ve conquered the first week of breastfeeding! Hopefully you’ve learned your baby’s feeding cues, mastered the latch, and established a breastfeeding routine, but if not don’t be discouraged. It’ll come soon.
Supportive Network: Having a strong support system can make all the difference. Consider connecting with a lactation consultant (IBCLC) or joining a breastfeeding support group. These professionals can offer valuable guidance on troubleshooting any challenges you may face.
Additional Support: Hygeia is also here for you! We offer a hospital-grade strength breast pump designed to mimic a baby’s natural suckling pattern for efficient milk expression.
Remember, mama, you are doing an amazing job! Breastfeeding is a beautiful and rewarding experience. By following these tips, seeking support when needed, and utilizing the right tools, you’ll be well on your way to a successful breastfeeding journey.

Breastfeeding latch may be natural, but that doesn’t guarantee the initial latching process will come naturally–for you or baby. Achieving that successful latch can sometimes feel like a complex enigma, especially for new moms. However, it’s an essential step in achieving fruitful breastfeeding goals. A strong latch will guarantee your comfort as well as your baby’s ability to fill up on milk effectively.
This quick guide will equip you with the knowledge and strategies to master the art of the breastfeeding latch, setting you and your baby on the path to a smooth and joyful breastfeeding journey.
Why is a Good Latch Important?
A proper latch ensures your baby receives the nutritious hindmilk, the fattier milk that comes after the initial foremilk. That’s not to mention that a good latch helps prevent nipple pain, promotes milk production, and reduces the risk of blocked ducts and mastitis.
Signs of a Good Latch:
Wide Mouth Opening: Your baby’s mouth should be wide open, with a good portion of your areola (the darker area around the nipple) visible above their upper lip.
Deep Latch: Your baby’s chin should be resting on your breast, and their lips flanged outward, forming a seal around your areola.
Comfortable Feeding: You shouldn’t experience any nipple pain during feeding. You may feel a tugging sensation, but it shouldn’t be sharp or uncomfortable.
Effective Swallowing: Observe your baby swallowing regularly during feeding, with pauses in between sucks.
Strategies for Achieving a Good Latch:
Skin-to-Skin Contact: Initiate feeding with skin-to-skin contact. This not only promotes bonding but also encourages your baby to root and latch on instinctively.
Support Your Breast: Use a C-hold (thumb on top and fingers cupping underneath) to support your breast without blocking your baby’s nose.
Tickle and Trigger: Gently tickle your baby’s lips with your nipple to stimulate their rooting reflex. Wait for them to open their mouth wide before offering your breast.
Aim High: Aim your nipple towards the roof of your baby’s mouth, not just the tip.
Observe and Adjust: Pay close attention to your baby’s cues and adjust your positioning or latch if needed. Don’t be afraid to seek help from a lactation consultant if you’re struggling.
Common Latch Challenges and Solutions:
Shallow Latch: If your baby isn’t latching deeply enough, try unlatching them and repeating the steps above, ensuring they take a bigger mouthful of breast tissue.
Tongue Tie: Ankyloglossia, or tongue tie, can restrict your baby’s tongue movement and make latching difficult. Consult your doctor or a lactation consultant to discuss if a frenotomy (tongue-tie release) is the right solution.
Flat or Inverted Nipples: While flat or inverted nipples can pose a challenge initially, they don’t necessarily prevent successful breastfeeding. There are techniques and tools like nipple shields that can help your baby latch.
Supporting Your Breastfeeding Journey Every Step of the Way
At Hygeia Health, empowering mothers on their breastfeeding journeys is our priority. While breast pumps may be our specialty, we understand the importance of a good latch and offer a variety of resources to support you, including:
Informative blog posts: Our blog is packed with valuable information on various breastfeeding topics, including latching techniques.
Insurance-covered lactation consultations: We can connect you with a lactation consultant who can provide personalized guidance and support. Click here to learn more about Hygeia Health’s breastfeeding resources and insurance-covered lactation consultations!
Embrace the joy of breastfeeding with a confident latch and the support you deserve!

Breastfeeding is a beautiful journey, but it can also come with challenges, especially in those early days. Finding a comfortable and successful latch is key for both you and your baby. The good news is, there’s no single “right” position – every mom-baby pair finds what works best breastfeeding position.
Popular breastfeeding positions to get you started:
- The Cradle Hold: This classic position is a great go-to for many moms, particularly newborns. You cradle your baby close, arm supporting their head and neck, with their body facing yours. Their tummy should be against yours, promoting skin-to-skin contact. This position allows for easy control and good visibility to ensure a proper latch.
- The Cross-Cradle Hold: Similar to the cradle hold, but with your baby nestled across your body, supported by the opposite arm. This can be helpful for babies with torticollis (a stiff neck) or those who have trouble turning their heads towards one breast.
- The Football Hold: This hold is like a quarterback cradling a football under their arm. Perfect for newborns with latching difficulties or moms with larger breasts. With your baby tucked under your arm, their head resting near your breast, it allows for better control and deeper latching.
- The Side-Lying Position: This cozy position is ideal for nighttime feedings or relaxed lounging. Lie on your side facing your baby, with pillows for support. Your baby can then nuzzle in close, latching comfortably.
- The Laid-Back Position: This relaxed approach allows gravity to assist your baby in latching. Recline comfortably, with your baby lying on your tummy. Let your baby lead the way, rooting around and latching on naturally.
Tips for Success:
Comfort is Key: Experiment with different positions until you find one that feels natural and supportive for both you and your baby.
Proper Latch: Ensure your baby’s mouth is wide open and they have a deep latch on both the nipple and surrounding areola.
Support: Pillows can be your best friend for positioning and comfort. Use them to prop up your arms, support your back, or elevate your baby.
Skin-to-Skin Contact: This is essential for promoting bonding, regulating baby’s temperature, and improving milk production.
Finding the Perfect Fit:
While breastfeeding positions are crucial, having the right breast pump can also play a significant role in your breastfeeding journey. Hygeia Health offers a range of high-quality breast pumps designed for comfort, efficiency, and discreet pumping.
Ready to Apply for a Free Breast Pump?
Many insurance companies are required to cover the cost of a breast pump under the Affordable Care Act. Hygeia Health can help you navigate the insurance process and determine if you qualify for a free breast pump through our simple online application. Visit our website at Hygeia Health website to get started today!
By finding a comfortable breastfeeding position and having the right support system in place, you can embark on a successful and rewarding breastfeeding journey.