The most common word used to describe breastfeeding is “natural”. This act shared between mother and baby reflects the beauty found in the natural role of motherhood. “Natural” also reflects why breastfeeding needs prioritized in today’s world. Breastfeeding is a natural solution and therefore a sustainable one. World Breastfeeding Week 2025 inspires us to look beyond the immediate act of feeding and consider a much bigger picture. This blog post will dive into the this year’s theme: “Prioritize Breastfeeding: Create sustainable support systems.”
The Environmental Toll of Artificial Feeding
Hygeia is in full support of all mother’s and how they choose to feed their babies, be it breastfeeding or formula. Fed is best. No questions. This is truly the most important thing for every baby and that every mom knows what is best for her and her baby.
However, it is important to recognize that the environmental impact of artificial feeding is considerable. The entire process of formula production is energy-intensive and resource-heavy. From sourcing ingredients to manufacturing, packaging, and global distribution, it is a far cry from a “natural renewable food” like breast milk. One one hand, breast milk is environmentally safe and produced and delivered to the consumer without pollution, packaging, or waste. Artificial milk options demand significant amounts of electricity, fuel for transportation, and water for processing and cleaning. The waste generated, from non-recyclable containers to discarded formula, places a heavy burden on our planet’s ecosystems.
Building Sustainable Support Systems
Recognizing breastfeeding’s vital role in a sustainable future isn’t enough. We must create robust and sustainable support systems for families. There are numerous ways this can be done.
- Community Support: Grass roots is where all things begin. Fostering networks of lactation consultants, peer support groups, and family encouragement are necessary for normalizing breastfeeding. At Hygeia, we offer lactation support in partnership with Nest Collaborative. These virtual breastfeeding consults are accessible anytime, anywhere, and covered by most insurance plans.
- Workplace Policies: For breastfeeding to be normalized there must be support in the workplace. This will happen through advocacy for comprehensive paid maternity leave and flexible work arrangements. Additionally, moms need dedicated breastfeeding-friendly environments with clean, private lactation spaces.
- Healthcare System: The support and education must begin from day one for mothers. We must ensure that healthcare providers are well-trained in lactation support. Facilities must also adhere to best practices like the Baby-Friendly Hospital Initiative.
- Policy and Advocacy: Globally, we must endorse policies that protect, promote, and support breastfeeding. This includes strict adherence to the International Code of Marketing of Breast-milk Substitutes to counter misleading marketing.
- Changing the Narrative: All of these steps will play a part, but individuals must also work to normalize breastfeeding in all settings. Encourage a mom who is breastfeeding in public. Educate a friend on her public breastfeeding rights. Help dismantle any lingering stigma around breastfeeding.
Breastfeed
At Hygeia, we believe that empowering mothers is the first step toward a more sustainable future. By providing you with access to our high-quality breast pumps, we aim to make breastfeeding a comfortable and efficient experience. Every journey is unique, which is why we’re dedicated to helping you get your pump 100% covered by your insurance plan. We are removing financial barriers to this natural choice.
Supporting a mother is an act of environmental stewardship. By strengthening the systems around us—from our communities to our workplaces—we can make breastfeeding a realistic option for more families. It’s an investment in a healthier tomorrow, for our children and for our planet. Therefore, join us in championing this natural, sustainable solution during World Breastfeeding Week.

Imagine a single act that nourishes a baby, empowers a mother, and protects our planet. This World Breastfeeding Week 2025, we’re doing more than celebrating infant feeding; we’re championing a powerful solution for our planet’s future. From August 1st to 7th, the #WBW2025 campaign will shine a crucial spotlight on the profound connection between breastfeeding, environment, and climate change, urging all to “Prioritize Breastfeeding: Create Sustainable Support Systems.”
The world is in the trenches of era where environmental concerns dominate global conversations. Hygeia will always support mothers in finding the best solution for their personal situation and seeing to it that baby is fed and mother is healthy. However, at Hygeia, we also know it is vital to recognize breastfeeding as a key player in fostering a sustainable environment and actively reducing the impact of climate change caused by artificial feeding.
The Green Power of Breastfeeding
Breast milk is often called nature’s perfect food, but its environmental benefits are equally remarkable.
Reduced Carbon Footprint
Unlike infant formula, breastfeeding boasts a significantly lower carbon footprint. It requires no industrial manufacturing processes, factories, or energy-intensive machinery that release greenhouse gas emissions. Furthermore, breast milk is the ultimate local food; it requires no transportation, eliminating the emissions associated with shipping ingredients or finished products across vast distances.
Waste Reduction
Breastfeeding is a champion of waste reduction. It produces absolutely zero waste – no plastic bottles, no metal cans, no paper packaging to end up in landfills. Breastfeeding also significantly reduces water consumption. There’s no need for water to prepare formula or sterilize bottles, conserving this precious resource. While a breastfeeding mother needs to stay hydrated, this is a natural biological need, not an industrial demand.
Conservation of Resources
Breastfeeding lessens our reliance on industrial agriculture, particularly the dairy industry. Most formulas are cow’s milk-based, an industry known for its contribution to methane emissions from livestock, extensive land degradation for grazing, and massive water usage. By choosing breastfeeding, we indirectly support resource conservation and the protection of biodiversity, promoting more sustainable practices overall.
Championing the Natural Solution
This World Breastfeeding Week 2025, let’s come together to champion this incredible, natural solution. At Hygeia Health, we are dedicated to empowering mothers through high-quality breast pumps and comprehensive support. Our products are designed to make breastfeeding more comfortable and efficient, while our resources provide valuable information and guidance.
By prioritizing breastfeeding and building strong, lasting support systems, we’re not just investing in the health and well-being of our children; we’re taking meaningful climate action and fostering a truly sustainable environment for future generations. Every ounce of breast milk is a drop in the ocean of positive change.

Pregnancy and postpartum are journeys filled with immense joy and a whirlwind of emotions. While you’re likely busy preparing for your new arrival, it’s crucial to prioritize your own well-being. This includes your mental health, which can sometimes take a backseat during these demanding yet beautiful times.
Understanding the Landscape: Common Mental Health Concerns
Many women experience emotional shifts during pregnancy and postpartum. Some of the most common concerns include:
Anxiety: Worrying about the health of your baby, labor and delivery, or parenthood in general is perfectly normal. However, if anxiety becomes overwhelming and interferes with your daily life, it’s important to seek help.
Depression: Feeling down, low on energy, or experiencing a loss of interest in activities you once enjoyed could be signs of perinatal depression, which affects millions of women.
Baby Blues: Feeling weepy, irritable, or overwhelmed in the first few days after delivery is common. If these feelings persist beyond two weeks, it could be a sign of postpartum depression.
Postpartum OCD (Obsessive-Compulsive Disorder): Intrusive thoughts or repetitive behaviors centered around your baby’s well-being can be a sign of postpartum OCD.
It’s Okay to Ask for Help: Resources and Strategies
The good news is that you don’t have to navigate these challenges alone. Here are some resources and strategies to support your mental well-being:
Talk to Your Doctor: Be open and honest with your doctor about your emotional state. They can screen for perinatal mood and anxiety disorders and recommend treatment options.
Connect with a Therapist: Therapy can provide a safe space to explore your feelings and develop coping mechanisms. Consider therapists specializing in perinatal mental health. There are many options to search for therapists, including the Psychology Today website, where you can filter on geography and area of focus, and then read biographies of therapists in your area.
Support Groups: Connecting with other mothers experiencing similar challenges can be incredibly validating. Online and in-person support groups can be a source of strength and connection.
Self-Care Practices: Prioritize activities that nourish your mind and body, such as meditation, yoga, spending time in nature, or pursuing hobbies you enjoy.
Building a Strong Support System: Having a reliable network of family, friends, or a partner who can listen and offer support can make a significant difference.
Hygeia Cares: Supporting Moms Every Step of the Way
At Hygeia Health, we understand that motherhood is a journey with its unique set of challenges and rewards. We’re committed to empowering mothers not just with high-quality breast pumps, but also with resources for your overall well-being.
Here are some additional resources we recommend:
- The National Maternal Mental Health Hotline: Call or text 1-833-TLC-MAMA (1-833-852-6262) for confidential support from trained counselors, available 24/7.
- Postpartum Support International (PSI): Offers support groups, resources, and a helpline (Postpartum Support International).
Remember, prioritizing your mental health is not a sign of weakness – it’s a sign of strength and a commitment to your well-being. By seeking support and taking care of yourself, you’ll be better equipped to care for your baby and thrive in your new role as a mother.

October is Breast Cancer Awareness Month, a time to raise awareness about this serious disease that has impacted nearly all of our lives in one way or another. Breastfeeding has been linked to a reduced risk of breast cancer, making it an important topic for women of all ages, but there is more to know about early detection and risk factors.
What is breast cancer?
Breast cancer is a disease that occurs when cells in the breast grow abnormally and divide uncontrollably. It can affect both men and women, but it is most common in women. It can occur at any age but it is seen in women above the age of 40 years most frequently.
Do you know the signs and symptoms?
Early detection is key to successful treatment of breast cancer. If you notice any of the following changes in your breasts, see your doctor:
- A lump or thickening in the breast or underarm
- A change in the size, shape, or texture of the breast
- Nipple discharge (other than breast milk)
- Skin changes on the breast, such as dimpling, puckering, or redness
- Pain in the breast
What are the risk factors?
Several factors can increase your risk of developing breast cancer, including:
- Age: The risk of breast cancer increases with age
- Family history: Having a close relative with breast cancer can increase your risk.
- Genetics: Certain genetic mutations, such as BRCA1 and BRCA2, can increase your risk.
- Hormone therapy: Taking hormone replacement therapy after menopause can increase your risk.
- Breast lumps: Women who have had some type of non-cancerous breast lumps are more likely to develop cancer later on.
- Dense breast tissue: Women with dense breast tissue have a higher chance of developing breast cancer.
- Obesity: Being overweight or obese can increase your risk.
- Diet & Lifestyle choices: Women who smoke, eat a high-fat diet, and drink alcohol are more at risk of developing breast cancer.
- Radiation exposure: Frequent exposure to X-rays and CT scans may raise a woman’s chance of developing breast cancer.
Breastfeeding and Breast Cancer
Studies have shown that breastfeeding can reduce your risk of developing breast cancer. The longer you breastfeed, the greater the protection.
At Hygeia Health, we believe in the power of breastfeeding. Our high-quality breast pumps are designed to make pumping easier and more efficient, allowing you to focus on bonding with your baby.
We also offer resources and support to help mothers on their breastfeeding journey. Our website provides information on breastfeeding and pumping, and our customer service team is available to answer your questions.
Get a Free Breast Pump
We believe that every mother should have access to the tools and support they need to breastfeed their baby. That’s why we offer 100% insurance-covered breast pumps to mothers who are breastfeeding or have recently breastfed.
To apply for a free breast pump, simply visit our website and fill out the application form. We’ll review your application and contact you with the next steps.
Empower Yourself
By understanding the risks of breast cancer and the benefits of breastfeeding, you can take steps to protect your health. Schedule regular check-ups with your doctor, perform monthly self-exams, and consider genetic testing if you have a family history of breast cancer.
Let’s work together to raise awareness about breast cancer and support those affected.

Breastfeeding is a beautiful journey that nourishes your baby with the perfect blend of nutrients and antibodies. But for busy moms, pumping allows for flexibility and convenience, ensuring your baby receives the benefits of breastmilk even when you’re not there.
Whether you’re a seasoned pumping pro or just starting out, mastering the process of pumping, storing, thawing, and feeding breastmilk empowers you to confidently navigate your breastfeeding journey. Here’s your comprehensive guide:
Pumping Essentials:
Find Your Rhythm: Establish a pumping routine that works for you. It could be several short sessions throughout the day or longer stretches that fit your schedule. Consistency is key to maintaining milk supply.
Choosing Your Pump: A high-quality breast pump makes a world of difference. Hygeia Health offers a comfortable, efficient, and quiet hospital-grade pump that is free to many through insurance. Consider your needs – portability for on-the-go pumping or a hospital-grade option for frequent pumping sessions.
Perfect Latch & Positioning: Proper positioning and latch ensure optimal milk flow and prevent discomfort. Your baby’s mouth should be wide open, with their chin and lower lip flanged outward. Their tongue should be positioned over a large portion of your nipple and most of the darker area around your nipple, called the areola). This ensures they get enough milk and prevents nipple pain for you. If you’re unsure about your latch, don’t hesitate to ask a lactation consultant for help.
Storing Liquid Gold: Safeguarding Your Breast Milk
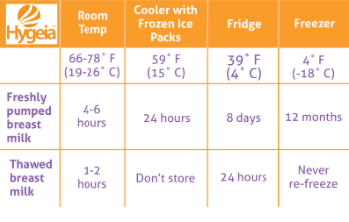
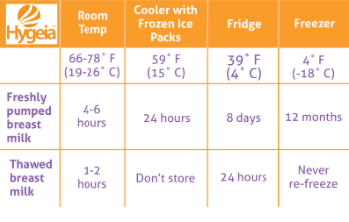
Fresh is Best: Freshly pumped breast milk can be stored at room temperature (up to 77°F) for up to 4 hours. This is ideal for short outings or pumping between nursing sessions.
Refrigerator Storage for Later: For longer storage, refrigerate breast milk in the back of the refrigerator where the temperature is most stable. Properly stored milk can last up to 4 days.
Deep Freeze for Long-Term Storage: Breast milk can be stored in the deep freezer (at 0°F or below) for up to 12 months. However, milk quality can degrade over time. Label containers with the date to ensure you use the oldest milk first.
Adding to your Storage: Small amounts of expressed milk may be added to the same refrigerated container or even a frozen container. The key is that the milk you want to add is cooled in the fridge beforehand. Don’t add body-temperature milk to cooled or already frozen milk.
Hygeia’s Storage Solutions: Invest in high-quality breast milk storage bags or containers. Hygeia Health offers a range of leak-proof, BPA-free storage options to keep your precious milk safe, including a cooler bag for temporary storage on the go.
Thawing Treasures: Warming Up Breast Milk Safely
Never Microwave: Don’t even think about it. Not only does microwaving destroy nutrients in breast milk but it can also create hot spots that could burn your baby’s mouth.
Gradual Thawing: The safest method is to thaw frozen breast milk in the refrigerator overnight or generally 12 hours. For quicker thawing, place the sealed milk bag or container in a container of lukewarm water, but never in boiling water. This kind of heat can damage the nutrients. It is also important to not let it thaw at room temperature.
Temperature Check and mixing: Before feeding, test a drop of milk on the inside of your wrist to ensure it’s lukewarm, not hot. Be sure to swirl the milk in the bag or bottle as the milk can separate during storage and you want to blend all the fats.
Limited window: Once you’ve thawed milk and left it at room temperature, you want to feed it to your baby within two hours. If that doesn’t happen, do not refreeze the milk. It’s time to pitch.
Feeding Time! Delivering the Goodness
Room Temperature or Chilled?: Either is fine! Breast milk can be fed to your baby at room temperature or chilled. Some babies may even prefer cooler milk. You can also warm the milk to body temperature but it’s not necessary.
Fresh vs. Thawed: If possible, prioritize using fresh or refrigerated breast milk over thawed milk. Thawed milk may have a slightly different taste or smell. It’s still perfectly safe for your baby; however, it will store longer and you can’t refreeze it once thawed, so save it for later.
Bottles and Nipples: Choose bottles designed for breastfed babies to help prevent nipple confusion. Experiment with different nipple types to find one your baby takes comfortably.
Hygeia’s Feeding Accessories: Hygeia Health offers a variety of bottle and nipple options to ensure a smooth transition between breast and bottle feeding.
Embrace the Journey with Hygeia Health
Juggling motherhood and breastfeeding can be demanding, but pumping empowers you to provide your baby with the irreplaceable benefits of breast milk. Hygeia Health is here to support you every step of the way.
We offer a convenient insurance-covered breast pump program to eligible mothers. Our hospital-grade pump is designed for comfort, efficiency, and portability, making it perfect for busy moms.
Click here to apply for your free breast milk pump today!
With the right knowledge, tools, and support system, you can confidently navigate pumping, storing, thawing, and feeding breast milk. Happy pumping, mamas!