Pregnancy is a wild ride, and your body is in for quite a transformation. One of the biggest changes you’ll notice is how your breasts grow and change. Pregnancy brings incredible changes to your body, including how your breast change during pregnancy and breastfeeding. Maybe you’re up for that; maybe you dread it. Either way, understanding what’s going on can help you feel more comfortable and ready for the journey ahead.
Physical Changes
As your body adapts to the demands of pregnancy, you’ll notice significant changes in your breasts. From increased sensitivity to the production of colostrum, these changes are all part of a natural process that prepares you for breastfeeding. Let’s first take a closer look at how these changes progress.
Hormonal Changes: Not the pregnancy hormones! Actually, these hormones are exactly what your body needs. During pregnancy, your body produces increased levels of estrogen and progesterone. These hormones play a role in uterine growth, placenta formation, and, you guessed it, breast growth.
Increased Blood Flow: Worried about your sensitive breasts? Don’t be! It’s completely normal. It’s often something that tips off a mom to her pregnancy before she’s even taken a test. As your breasts grow, they require more blood flow to support their development. This increased blood flow can sometimes cause your breasts to feel tender or sensitive.
Milk Ducts: The milk doesn’t just show up along with your baby. During pregnancy, your body begins to develop milk ducts. These ducts are tiny tubes that carry milk from the milk-producing glands to your nipples. While they will develop during your pregnancy, it will be the routine breastfeeding and/or pumping that will maintain them after delivery.
Colostrum: Get ready for liquid gold! In the later stages of pregnancy, you may begin to produce colostrum. Colostrum is a thick, yellow fluid that is rich in nutrients and antibodies. It is the first milk that your baby will receive after birth, so it’s good news if you notice it in the final days of pregnancy.
Preparing for Breastfeeding
It is important to take care of your breasts during pregnancy to prepare for breastfeeding. Here are a few tips:
Wear supportive bras: As your breasts grow, it is important to wear bras that provide adequate support. You not only want comfort for you, but the best support for your growing and changing breasts.
Massage your breasts: Gently massaging your breasts can help stimulate milk production and improve your milk flow. This can also help prevent clogged milk ducts.
Learn about breastfeeding: Taking a breastfeeding class or reading books about breastfeeding can help you feel more prepared. While your phone may be able to answer anything on the spot, it’s best to already have reliable resources in a pinch.
Embrace the Changes
Pregnancy is a time of incredible change. By understanding the changes that your breasts are going through, you can feel more prepared and confident for breastfeeding.
At Hygeia Health, we understand the importance of breastfeeding and the challenges that mothers may face. Our high-quality breast pumps are designed to make pumping easier and more efficient, allowing you to focus on bonding with your baby.
We also offer resources and support to help mothers on their breastfeeding journey. Our website provides information on breastfeeding and pumping, and our customer service team is available to answer your questions.
Get a Free Breast Pump
We believe that every mother should have access to the tools and support they need to breastfeed their baby. To apply for a free breast pump, simply visit our website and fill out the application form. We’ll review your application and contact you with the next steps.

Breastfeeding is a beautiful journey, but the idea that it’s completely “free” can be a little misleading—especially if you plan to pump. Between bottles, storage bags, accessories, and a quality breast pump, the costs can add up fast.
The good news? Many insurance plans cover the cost of a breast pump, often making it free for moms! At Hygeia Health, we’re here to simplify the process so you can focus on what matters most: your baby. Here’s everything you need to know about getting a free breast pump through insurance.
Step 1: Check Your Insurance Coverage
The first step is to review your insurance plan. Search for terms like “breast pump,” “lactation equipment,” or “maternity benefits.” If you’re unsure, call your insurance provider and ask directly what’s covered under your plan.
Pro Tip: Some insurance plans even allow you to get your breast pump before your baby is born, so be sure to ask about this option!
Step 2: Get a Prescription
Most insurance providers require a prescription from your healthcare provider to cover the cost of a breast pump. Thankfully, this step is straightforward. Your doctor or midwife simply needs to confirm your pregnancy and recommend a pump.
Don’t hesitate to bring this up during your next prenatal visit—it’s a routine request and takes just a few minutes.
Step 3: Choose the Right Breast Pump for You
Choosing the right breast pump is essential for a smooth breastfeeding journey. With so many options on the market—manual, electric, hands-free, or hospital-strength—it’s important to pick one that matches your lifestyle and needs.
At Hygeia Health, we offer high-quality, hospital-grade breast pumps that are portable, eco-friendly, and easy to use. Whether you’re pumping at work, on the go, or at home, we’ve got the perfect pump for you. Apply for your pump here.
Step 4: Submit Your Claim
Once you’ve selected your breast pump, it’s time to submit a claim to your insurance provider. Here’s what you’ll likely need:
- A copy of your prescription
- Your breast pump receipt
- Any additional documentation required by your insurance
Don’t worry—if you need help with this step, Hygeia Health is here to guide you through it.
Step 5: Know Your Rights
Under the Affordable Care Act, most insurance plans are required to cover breastfeeding equipment, including breast pumps. If you encounter any hurdles with your insurance provider, remember that you have rights as a breastfeeding mom.
Advocate for yourself, and don’t hesitate to reach out to Hygeia Health for support.
How Hygeia Health Makes It Easy
We know insurance paperwork can feel overwhelming, especially for expectant moms juggling a million other tasks. That’s why Hygeia Health goes the extra mile to make this process as easy as possible.
Here’s how we help:
Insurance Assistance: Our team works with you to navigate the coverage process.
Hospital-Grade Pumps: All our pumps deliver top-tier performance and are covered by many insurance plans.
Fast & Simple Process: Get your pump quickly so you can focus on your baby.
Invest in Your Baby’s Health
Breastfeeding is one of the best investments you can make in your baby’s health and development. Don’t let cost—or paperwork—stand in the way. Hygeia Health is here to help you take full advantage of your insurance benefits and start your breastfeeding journey with confidence.
Apply for your free breast pump now and experience the Hygeia Health difference!

Amidst the excitement and anticipation of your pregnancy, you are more than likely to encounter a sea of well-meaning advice and information, not all of which is accurate. This is especially true when it comes to breastfeeding. Breastfeeding is a beautiful and natural way to nourish your baby, providing them with essential nutrients and antibodies for a healthy start. However, the benefits and naturalness of breastfeeding lead to some tall tales about its powers and ease. These tall tales are often referred to as “breastfeeding myths.”
Let’s bust some common breastfeeding myths and empower you to navigate your breastfeeding journey with confidence:
Myth 1: Breastfeeding is easy and natural.
While breastfeeding is a natural instinct, it doesn’t always come easily. Learning proper latching, establishing a routine, and managing potential challenges can take time and practice for both you and your baby. Don’t be discouraged if it takes a few tries – seek support from lactation consultants, nurses, or experienced mothers to overcome initial hurdles. You can schedule an appointment with a lactation consultant here.
Myth 2: Sore nipples are inevitable.
While some initial discomfort is common, especially in the first few days, ongoing pain is not normal. Ensure your baby is latching correctly, as a poor latch can lead to nipple soreness, and even bleeding. If you experience persistent pain, consult a lactation consultant for guidance on positioning and latch techniques.
Myth 3: You need to wash your nipples before every feeding.
Washing your nipples with soap before each feeding is unnecessary and can even disrupt the natural protective oils on your skin. Your baby benefits from the natural bacteria on your breasts, which helps build their immune system.
Myth 4: You can’t breastfeed if you have flat or inverted nipples.
Flat or inverted nipples can make latching more challenging, but it doesn’t mean you can’t breastfeed. With the help of a lactation consultant, you can learn techniques like nipple shields or positioning strategies to ensure successful breastfeeding.
Myth 5: Your breast size determines your milk supply.
Breast size has little to do with milk production. Your body produces milk based on the frequency and duration of your baby’s feeding, not the size of your breasts. The more your baby feeds, the more milk your body will produce to meet their needs.
Myth 6: You need to follow a strict diet while breastfeeding.
While a healthy diet is important for overall well-being, there’s no need for drastic dietary changes while breastfeeding. Focus on a balanced diet that includes fruits, vegetables, whole grains, and lean protein. Most foods won’t affect your milk supply or harm your baby.
Myth 7: Formula is just as good as breast milk.
While formula can be a safe and necessary alternative in some cases, breast milk provides unmatched benefits for your baby’s health and development. It contains essential nutrients, antibodies, and immune-boosting factors that formula cannot replicate. Your breastmilk will even naturally change and adapt to your baby’s needs.
Myth 8: You can’t breastfeed if you’re taking medication.
Most medications are compatible with breastfeeding. Consult your doctor to discuss any concerns and ensure you’re taking medications that are safe for both you and your baby.
Myth 9: You have to breastfeed on demand, even at night.
It is true that baby will, most likely, wake often during the night, especially in the early weeks. While frequent feeding is crucial for establishing milk supply, it’s okay to set boundaries and take breaks when needed. Your partner or a trusted caregiver can help with nighttime feedings to allow you some rest.
Myth 10: Breastfeeding is an all-or-nothing proposition.
Every breastfeeding journey looks different. Some mother’s choose to only feed at the breast while others solely pump and bottle feed. Others do a combination of the two. Even if you can’t exclusively breastfeed, every drop of breast milk your baby receives is beneficial. Combining breastfeeding with formula can still provide your baby with valuable nutrients and antibodies.
Remember, every breastfeeding journey is unique. Don’t hesitate to seek support from lactation consultants, healthcare professionals, and other breastfeeding mothers. Here’s a secret: most mothers do get help of some sort before they start feeling comfortable!
Hygeia Health is dedicated to supporting your breastfeeding journey. We offer a hospital-grade electric breast pump designed for comfort, efficiency, and portability, making it easier to express and store milk on the go.
Click here to learn how your insurance can cover the cost of our hospital strength pump and empower yourself to breastfeed with confidence!

Breastfeeding is a beautiful journey that nourishes your baby with the perfect blend of nutrients and antibodies. But for busy moms, pumping allows for flexibility and convenience, ensuring your baby receives the benefits of breastmilk even when you’re not there.
Whether you’re a seasoned pumping pro or just starting out, mastering the process of pumping, storing, thawing, and feeding breastmilk empowers you to confidently navigate your breastfeeding journey. Here’s your comprehensive guide:
Pumping Essentials:
Find Your Rhythm: Establish a pumping routine that works for you. It could be several short sessions throughout the day or longer stretches that fit your schedule. Consistency is key to maintaining milk supply.
Choosing Your Pump: A high-quality breast pump makes a world of difference. Hygeia Health offers a comfortable, efficient, and quiet hospital-grade pump that is free to many through insurance. Consider your needs – portability for on-the-go pumping or a hospital-grade option for frequent pumping sessions.
Perfect Latch & Positioning: Proper positioning and latch ensure optimal milk flow and prevent discomfort. Your baby’s mouth should be wide open, with their chin and lower lip flanged outward. Their tongue should be positioned over a large portion of your nipple and most of the darker area around your nipple, called the areola). This ensures they get enough milk and prevents nipple pain for you. If you’re unsure about your latch, don’t hesitate to ask a lactation consultant for help.
Storing Liquid Gold: Safeguarding Your Breast Milk
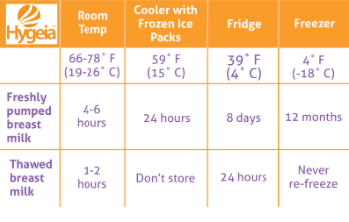
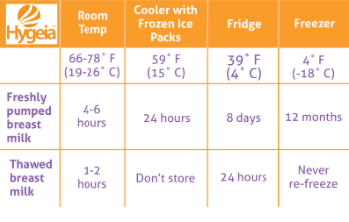
Fresh is Best: Freshly pumped breast milk can be stored at room temperature (up to 77°F) for up to 4 hours. This is ideal for short outings or pumping between nursing sessions.
Refrigerator Storage for Later: For longer storage, refrigerate breast milk in the back of the refrigerator where the temperature is most stable. Properly stored milk can last up to 4 days.
Deep Freeze for Long-Term Storage: Breast milk can be stored in the deep freezer (at 0°F or below) for up to 12 months. However, milk quality can degrade over time. Label containers with the date to ensure you use the oldest milk first.
Adding to your Storage: Small amounts of expressed milk may be added to the same refrigerated container or even a frozen container. The key is that the milk you want to add is cooled in the fridge beforehand. Don’t add body-temperature milk to cooled or already frozen milk.
Hygeia’s Storage Solutions: Invest in high-quality breast milk storage bags or containers. Hygeia Health offers a range of leak-proof, BPA-free storage options to keep your precious milk safe, including a cooler bag for temporary storage on the go.
Thawing Treasures: Warming Up Breast Milk Safely
Never Microwave: Don’t even think about it. Not only does microwaving destroy nutrients in breast milk but it can also create hot spots that could burn your baby’s mouth.
Gradual Thawing: The safest method is to thaw frozen breast milk in the refrigerator overnight or generally 12 hours. For quicker thawing, place the sealed milk bag or container in a container of lukewarm water, but never in boiling water. This kind of heat can damage the nutrients. It is also important to not let it thaw at room temperature.
Temperature Check and mixing: Before feeding, test a drop of milk on the inside of your wrist to ensure it’s lukewarm, not hot. Be sure to swirl the milk in the bag or bottle as the milk can separate during storage and you want to blend all the fats.
Limited window: Once you’ve thawed milk and left it at room temperature, you want to feed it to your baby within two hours. If that doesn’t happen, do not refreeze the milk. It’s time to pitch.
Feeding Time! Delivering the Goodness
Room Temperature or Chilled?: Either is fine! Breast milk can be fed to your baby at room temperature or chilled. Some babies may even prefer cooler milk. You can also warm the milk to body temperature but it’s not necessary.
Fresh vs. Thawed: If possible, prioritize using fresh or refrigerated breast milk over thawed milk. Thawed milk may have a slightly different taste or smell. It’s still perfectly safe for your baby; however, it will store longer and you can’t refreeze it once thawed, so save it for later.
Bottles and Nipples: Choose bottles designed for breastfed babies to help prevent nipple confusion. Experiment with different nipple types to find one your baby takes comfortably.
Hygeia’s Feeding Accessories: Hygeia Health offers a variety of bottle and nipple options to ensure a smooth transition between breast and bottle feeding.
Embrace the Journey with Hygeia Health
Juggling motherhood and breastfeeding can be demanding, but pumping empowers you to provide your baby with the irreplaceable benefits of breast milk. Hygeia Health is here to support you every step of the way.
We offer a convenient insurance-covered breast pump program to eligible mothers. Our hospital-grade pump is designed for comfort, efficiency, and portability, making it perfect for busy moms.
Click here to apply for your free breast milk pump today!
With the right knowledge, tools, and support system, you can confidently navigate pumping, storing, thawing, and feeding breast milk. Happy pumping, mamas!

Breastfeeding: it’s the way anyone can level up to supermom status, right?
While it is an amazing journey, it is completely normal to hit a few bumps in the road. The good news is no mom needs to be alone in their journey! There is a ton of support available to help moms navigate this new chapter of motherhood and empower them to thrive with breastfeeding.
In this blog post, in the spirit of World Breastfeeding Week, we will discuss the best people and places to find breastfeeding support.
Healthcare Providers
Your doctor or midwife is a great place to start for support. They may not be the experts themselves, but they can likely provide you with initial information, point you in a good direction for resources, and even refer you to lactation consultants. Remember, they deal with moms who are new to breastfeeding on a regular basis.
Lactation Consultants
Lactation consultants are specially trained professionals who can help with breastfeeding questions, problems, and general support. They are wonderful assets for assisting with latching, milk supply, and other common issues. Today, most hospitals have a lactation consultant on staff. If one does not visit you upon delivery, don’t miss out. Request that the on-staff lactation consultant visit before your stay is over.
Support Groups
A mom tends to feel less alone about her struggles when she’s able to share her experiences with others who are going through or have been through similar challenges..Support groups can be a great way to connect with other breastfeeding moms and get the encouragement needed. This can also be a great way to receive tips from moms who’ve had to tackle the same issues. La Leche League offers support groups across the country or check with your hospital, as many offer support groups. If yours does not, the lactation consultant may be aware of a local group.
Partners and Family
Your partner and family can, and hopefully will, play an important role in your breastfeeding journey. They can provide emotional support, help with household chores, and take care of older children if needed. Of course, not every mom has this kind of support at home. In this case, sometimes friend circles can become like family and set up meal trains and regular check-ins to be sure a mom has the support she needs.
Online Resources & Hygeia Health
The beauty of today’s world is that not everything has to be within driving distance to be accessible. There are many online resources available, including websites, blogs, forums, and even support groups. However, the plethora of options available can be both a blessing and a curse. An already overwhelmed mom struggling in her breastfeeding journey likely doesn’t have the fortitude to sift through endless search results. Fortunately, there are trustworthy sources for information, support, and community, such as La Leche League, Academy of Breastfeeding Medicine (ABM), Healthline and The World Health Organization (WHO).
Hygeia Health
We at Hygeia Health are on the top of the list as well! We’re here to support you in all ways. Our website offers information and resources on breastfeeding and our customer service team is available to answer your questions. We also partner with Nest Collaborative to provide virtual breastfeeding consults accessible anytime, anywhere, covered by most insurance plans at no cost to you.
Remember, you’re not alone. There are many people and resources available to help you on your breastfeeding journey. Don’t be afraid to ask for help.

Breastfeeding is a beautiful journey, but it’s not always easy. Many mothers face significant obstacles that can make breastfeeding challenging to sustain. This World Breastfeeding Week, we want to shed light on these struggles and obstacles and offer support. This blog post will dive into those challenges.
Physical Challenges
Sore nipples, engorgement, and mastitis–ever heard of those? These are some of the most common physical hurdles moms face. These can be incredibly painful and downright discouraging for a mom. No matter how much she understands the benefits of breastfeeding, the pain can cause a mom to want to give up or feel incapable. Lack of sleep in the early days and weeks after birth, coupled with the demands of a newborn, can further exacerbate these issues.
One of the major causes for physical challenges, though, is inadequate latching, which is often a result of a mom not being well supported after birth. This can be particularly true for a first time breastfeeding mom who doesn’t receive support from a lactation consultant. When breastfeeding support is lacking from the start, a mom can be quickly deterred.
Psychological Challenges
While the previously mentioned painful experiences of things like cracked and bleeding nipples may sound traumatic, physical challenges are often treated and managed more easily than the mental issues moms can face.
Feeling inadequate, stressed, or isolated is not an uncommon experience for breastfeeding mothers. The pressure to succeed can be overwhelming, especially when coupled with the mantra that “breastfeeding is natural”. The physical struggles coupled with the flood of hormones that follow delivery can result in postpartum depression and anxiety, which can further complicate the early breastfeeding journey.
Additionally, some moms struggle with body image concerns. Bodies obviously change through pregnancy, and, typically, they don’t simply “bounce back” to their pre-pregnancy shape, weight, and size. Living in a ‘new’ body can also lead to mental challenges for moms.
Societal and Environmental Challenges
Lack of workplace support is a major barrier for many mothers in their breastfeeding journey. Limited maternity leave, lack of lactation rooms, and negative attitudes towards breastfeeding can make it difficult for working moms to continue breastfeeding once returning to work.
Additionally, access to quality healthcare and lactation support is also crucial to breastfeeding success, and unfortunately, in many corners of the world ( even in the United States), not every mom has both or either of these things.
Other socioeconomic disparities can impact a mother’s ability to access these resources, such as income, education, geographic location, and racial/ethnic disparities. Discrimination can play a role for some, as can living in a rural or low income area.
Knowledge and Information Gaps
Misinformation about breastfeeding is prevalent. Many mothers lack the knowledge and support they need to overcome challenges and this can lead to early cessation of breastfeeding.
Hygeia Health is committed to supporting mothers on their breastfeeding journey. Our breast pumps are designed with comfort and efficiency in mind. But we know that a great breast pump is just one piece of the puzzle. We believe in providing comprehensive support, including education, resources, and community.
By understanding the challenges mothers face, we can work together to create a more supportive environment for breastfeeding. Let’s break down the barriers and continue to close the gap that will help mothers achieve their breastfeeding goals.